Medical cannabis has become an increasingly important treatment option since the UK legalised it in November 2018. Private clinics in England issued over 300,000 medical cannabis prescriptions – more than double the 150,527 recorded the year before. This rapid growth shows how many people are finding relief from conditions like chronic pain, epilepsy, and multiple sclerosis through medical marijuana.
However, as medical cannabis becomes more widely available, important questions emerge: How does addiction risk with medical cannabis compare to recreational use? Are patients who follow their doctor’s prescription still at risk? And what makes cannabis dependency different from other prescription drug dependencies? Understanding these nuances can help patients and families make informed decisions about cannabis addiction risks and cannabis rehab treatment.
The Short Answer: Yes, But It’s Complicated
While medical cannabis can help treat serious conditions, it does carry addiction risks – even when prescribed by doctors. The key difference from other medications is that medical cannabis often contains THC, the same compound that makes recreational cannabis psychoactive.
Professor Jonathan Chick, a leading addiction expert and former Medical Director at Castle Craig, explains: “Using cannabis as a medicine can lead to addiction. Some regular users will find it extremely difficult to reduce or stop their cannabis consumption despite being aware of increasing problems.”
Why Was Medical Marijuana Legalised?
On the 1st November 2018 the UK government changed the law to allow cannabis-based medical products to be prescribed for medical use. These medicines can only be prescribed by specialist doctors and must either be licensed, part of a clinical trial, or a “special” unlicensed medicine prescribed under strict rules. This marked a significant shift, allowing specialist doctors to prescribe cannabis-based medicinal products for conditions like chronic pain, epilepsy, and multiple sclerosis, while keeping recreational cannabis use and unsupervised self-administration prohibited.
This decision was spurred by evolving public attitudes and scientific evidence supporting cannabis’s efficacy for conditions like Alzheimer’s, cancer-related pain, chronic pain, multiple sclerosis, and Crohn’s disease. High-profile campaigns, particularly for children with epilepsy, underscored the need for legal access to CBMPs when conventional treatments failed. The National Institute for Health and Care Excellence (NICE) continues to provide guidelines, emphasising that medical cannabis is a last-resort treatment.
Cannabis-based products licensed in the UK by the National Institute for Health and Care Excellence (NICE) include:
- Sativex (THC combined with CBD) for multiple sclerosis spasticity
- Nabilone for severe nausea from chemotherapy
- Pure CBD products like Epidiolex for certain types of epilepsy
- Synthetic THC compounds like dronabinol.
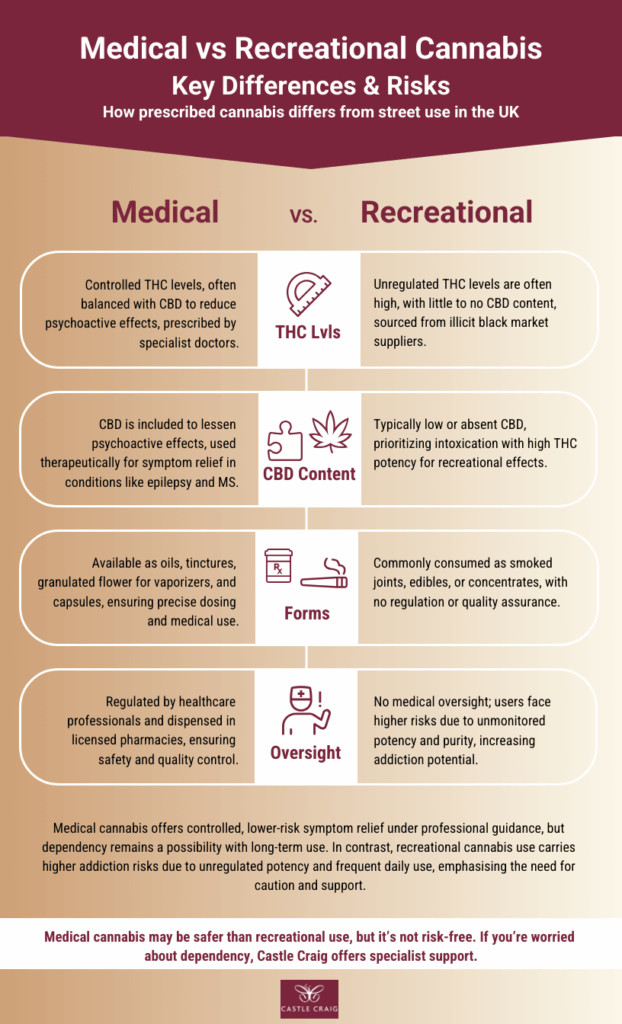
Medical cannabis in the UK may be prescribed in different forms – from oils and tinctures to granulated flower for vaporisation – but only when prescribed by a specialist doctor.
Market Growth: Medical Cannabis
In 2025, approximately 80,000 UK patients are estimated to use medical cannabis, driven by growing acceptance and expanded private clinic access. In 2023, Statista reported that Europe’s medical cannabis market was worth about $745 million, and it is forecast to grow rapidly between 2023 and 2027 as more countries legalise its use.
The UK medical cannabis market is growing and is projected to reach £300 million in the UK by 2025, according to reports from the BBC. Yet questions remain about the impact on addiction rates and the wider medical community. With the UK’s drug advisory council urgently reviewing medical cannabis regulation, as rising prescriptions spark concerns over safety and dependency – how can the UK balance the benefits of medical cannabis with the risks of dependency? Are the risks of cannabis addiction recognised and what steps are being taken to mitigate these risks?
What Makes the Cannabis Plant Unique?
The cannabis plant contains more than 100 cannabinoids, with tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most studied. THC drives the psychoactive effects, while cannabidiol (CBD) is non-intoxicating and offers anti-inflammatory, anxiolytic, and anti-epileptic properties.
Unlike recreational cannabis, which is usually smoked or eaten, medical cannabis products are carefully formulated with controlled THC levels, often balanced with CBD to reduce unwanted psychoactive effects. This complexity means medical cannabis must be precisely prescribed to maximise therapeutic benefits while minimising risks.
Will Medical Cannabis Help?
Emerging studies in 2025 suggest promise for medical cannabis in treating anxiety, chronic pain, epilepsy, and even opioid addiction. For instance, CBD-based treatments like Epidiolex for epilepsy and Sativex for multiple sclerosis are now established options. However, addiction expert, Professor Jonathan Chick notes, “For severe conditions like treatment-resistant epilepsy, the benefit-to-risk ratio justifies cannabis use, but for less disabling conditions, the potential for side effects, including dependency, warrants caution.” The UK’s private clinic model has expanded access, but only a handful of NHS prescriptions are issued, highlighting the need for more robust clinical trials.
There are many questions that need to be considered in the legalisation of medical cannabis. For instance, how do we create the most effective medicine? Who can safely prescribe these medicines?
Who Can Prescribe Medical Marijuana in the UK?
In 2025, only specialist doctors on the General Medical Council’s Specialist Register can prescribe CBMPs, typically after patients have failed at least two conventional treatments. However, challenges persist: the lack of standardised formulations and limited high-quality research make doctors cautious. The UK’s Food Standards Agency launched a public consultation in August 2025 on three CBD food product applications (RP07, RP350, and RP427). If approved by ministers, these would become the first legally authorised CBD food products in Great Britain. Meanwhile, private prescriptions remain costly, and caution among medical professionals continues to limit adoption.
In Professor Chick’s view, “Few of the preparations have been subjected to safety testing in large numbers of patients. This is necessary to provide a licence that allows the doctor some legal protection if safety concerns emerge. There is a risk of unwanted effects when prescribing any drug i.e. new symptoms developing due to the cannabis. When medical cannabis is used for less disabling conditions, this risk might begin to outweigh the likelihood of benefits to the original symptoms. Thus, doctors will be more cautious.”
The Risk of Prescribed Cannabis Addiction
Unlike opioids or benzodiazepines, where physical dependence can be severe and withdrawal dangerous, cannabis dependency is more often psychological, particularly with long-term use. However, withdrawal symptoms such as anxiety, irritability, and sleep disturbance can still make stopping very difficult. A 2025 University of Bath study found that patients using cannabis to manage anxiety or depression reported higher overall consumption, which may increase the risk of dependency.
Most NHS treatment data refers to recreational cannabis use, but these patterns remain important when considering long-term prescribing risks. NHS data, for example, shows that in 2021–2022 around 21% of new entrants to drug treatment programmes cited cannabis as their primary issue, and treatment demand has continued to rise into 2025. Similarly, research highlights that adolescents who begin using cannabis at 14 or 15 are over three times more likely to develop severe cannabis use disorder – again based on recreational cannabis use patterns.
These findings are still relevant when considering prescribed cannabis, as dependency risk is strongly linked to frequency of use and THC potency. Daily use carries a dependency risk of up to 1 in 3, and withdrawal symptoms such as anxiety, irritability, and sleep disturbance can make it difficult to stop. Addiction risk is generally lower with prescribed cannabis than with recreational use, but dependency can still develop, especially with long-term or daily use.
“Using cannabis as a medicine can lead to addiction. Some regular users will find it extremely difficult to reduce or stop their cannabis consumption despite being aware of increasing problems. This is partly due to withdrawal symptoms such as anxiety and sleep disturbance when they try to cut down the cannabis intake. In addition, emotional difficulties may have been masked, or created, which they are used to ‘treating’ with cannabis. They simply don’t wish to stop. The rise in high-potency THC products exacerbates these risks, with links to cognitive impairment, memory issues, and, in young adults, increased psychosis risk.”
– Professor Jonathan Chick, MA (Cantab), MPhil, MBChB, DSc
Cannabis Policy in the UK: Decriminalisation vs Public Health Risks
The 2025 London Drugs Commission report recommends decriminalising personal possession of natural cannabis by moving it under the Psychoactive Substances Act, while retaining strong criminal penalties for supply and production. It advocates a harm-reduction and equity-based approach, emphasising better education, healthcare support, and addressing policing disparities – yet stops short of endorsing commercial legalisation due to lingering public health uncertainties. In response, the Royal College of Psychiatrists cautioned that even small daily amounts of natural cannabis or synthetic cannabinoids can significantly harm mental health, increasing the risks of depression, anxiety, and psychosis. They added: “As a priority, the UK Government must provide substance use and mental health services with the training, staff, and funding they need to support people with co-occurring substance use and mental illness.”
What This Means for Patients and Families
If you’re considering medical cannabis:
- Discuss addiction risks openly with your doctor
- Share any personal or family history of substance misuse and mental health concerns
- Understand that even prescribed cannabis use can lead to dependency
- Ask about lower-risk alternatives first.
If you’re currently using medical cannabis:
- Monitor your usage patterns honestly
- Be aware of signs of increasing tolerance (needing more for the same effect)
- Talk to your healthcare provider if you have any concerns about mood, anxiety, or sleep
- Remember that dependency can develop even with prescribed doses.
If you’re concerned about dependency:
- Seek professional support – effective treatment is available
- Know that recovery is absolutely possible with the right help and support is available at specialist clinics like Castle Craig.
A Last Word
Medical cannabis can be an effective treatment for serious conditions, but it’s not risk-free. Like many powerful medications, it can lead to dependency, especially with long-term use or in vulnerable individuals. Healthcare providers must prescribe cautiously, patients need honest education about risks, and families should be aware of warning signs.
If you’re struggling with cannabis dependency – whether from medical or recreational use – remember that effective, compassionate treatment is available. At facilities like Castle Craig, abstinence-based treatment programmes help people achieve long-term recovery in safe, therapeutic environments.
For more help about our specialist treatment programmes for cannabis addiction, you can contact us or request a call-back from a member of our admissions team.
References
- Cannabis-based Medicinal Products, NICE [accessed September 2025]
- BBC, Cannabis centre plans to ‘tap into global sector’ [accessed September 2025]
- Statista, Total medical cannabis market in Europe from 2023 to 2027 [accessed September 2025]
- The Guardian, Sadiq Khan calls for partial decriminalisation of cannabis possession, 28 May 2025 [accessed September 2025]
- RCPsych, Co-occurring substance use and mental health disorders (CoSUM), May 2025 [accessed September 2025]

